This will not be my most popular blog post ever.
You may not agree with me. That is okay. In fact, it is a good thing. If we all nodded our heads along to the beat of the same drum in this world, well, we would be a boring orchestra. Renza wrote a great piece on this notion recently, which can be found here.
One of the largest issues we face in the United States today is the “battle of the egos.” We see it play out on our Facebook newsfeeds each morning:
“I’m voting for so-and-so and I must be right because it’s my opinion and I said so and I can scream louder than you!!!”
Yes, we have a right to say such things. But do we really need to completely write off the other side of the opinion in the process? If we do, quite frankly, we are only hurting ourselves. Very rarely in life are issues so cut and dry, 100% right or wrong. When politics falls into the gray zone, which it so often does, our greatest hope for the best world possible is to hear and consider all opinions, to put aside our personal biases and to think about what truly matters. We are way too quick to judge.
“He looked like a thug. He must have done something wrong. He would have shot first.”
We do not always pause to think of the psychosocial reasons why he is in the wrong place at the wrong time, or why we are in the right place at the right time- safe from injury or premature death, judging from afar.
Or, we roll our eyes dismissively, choosing to believe a social media rant from someone who has never seen combat, or public service in a rough neighborhood:
“The cop had more than a split-second to make a life-or-death decision; his life, or the alleged suspect’s?! He doesn’t go home at night sick to his stomach about taking another’s life, whether or not the the law supports his defense…”
We do not always concede that maybe, just maybe, in this particular case, we are speaking of a human being who perhaps acted in fear, rather than hatred.
At one point or another, we are all guilty of not placing ourselves in the other’s shoes. It is easier for us to say that one side is 110% wrong, and we are 110% right. If only morals and ethics were so mathematically easy…
We do not always think about how unique individuals are, how we cannot check them off like bubbles on the SAT, fitting a prescribed correct answer to each situation. Maybe there is none. Let’s sit in the scariness of that idea, together. Let’s be more loving and considerate than we have been as a society in recent weeks.
Admittedly, I have been disappointed in the diabetes advocacy world for similar reasons of us not seeing all sides of the equation lately. There are days where the #doc rallies and we do something that is so obviously good: honoring Kycie Terry this month, for example.
Regularly, we laugh together, cry together, share our lives with diabetes together. This is what makes us tick, what gives a distinct purpose to this disease in which we are, despite it all, somehow able to rise above.
My concerns, though, echo Tom Goffe’s wonderful post regarding the impending FDA decision on potentially dosing insulin based on Dexcom continuous glucose monitors (CGMs).
***(Disclaimer: I am not a medical professional; do NOT consider any of this blog post to be medical advice intended for treatment purposes.)
My personal opinion on diabetes management is more of a Libertarian view, if we want to talk politics. I am perfectly okay with individual patient-centricity in disease management. Diabetes falls on a spectrum of manifestations; what works for me, may not work for you, and vice versa. If you want to dose according to Dexcom and you are comfortable doing so, by all means, that is your prerogative, and I truly wish you all the success in the world.
Although I no longer use an insulin pump due to a freaky product defect hullabaloo that I encountered, I am happy for all of those who still have access and great results from insulin pump technology. That same mindset goes for those who experience phenomenal Dexcom CGM accuracy and ease of dosing insulin accordingly.
Every great innovation in society has come by those who are brave enough to take risks. Think no further than the Open APS and #wearenotwaiting folks in our own community. Their courage, creativity, and selflessness are beyond measure.
My #DoseWithCGM worry, though, begins with this being a rushed decision. CGM technology is not quite there yet in my opinion, and to have a trusted federal agency say that it is- under pressure from one side of the equation, rather than all sides- is a slippery slope.
Dexcom is- again, in my own opinion- the most innovative diabetes company in the market right now; I am absolutely confident that their technology will only go up from here; but we should not compromise safety and swap out access to other products in the interim. Generally-speaking, the government can curtail efficiency in health tech, but this is one rare occasion where it serves as a proper check and balance. As far as CGM dosing, don’t ask, don’t tell; do whatever you want (as an informed, experienced, safety-focused patient), but leave the government out of it.
There are the obvious physical dangers to insulin dosing, at any time and using any product as a baseline judge of BG; diabetes can be a conniving JerkFace.
Sure, I have 25 years of T1D under my belt and have a good sense of the disparities between my CGM’s interstitial fluid reading, and the blood sugar reading of my meter. But what about a newly-diagnosed family? What if Mom boluses 7-year-old Jenny based off of the CGM’s 300, when she is really 180? What if she is advised that this is an appropriate treatment approach by a federal agency set in place to keep her safe?
Sadly, insulin can be as life-taking as it can be life-preserving, and the reality is that it can sway from either extreme quickly and easily- through no fault of the patient’s or caregiver’s. This disease has a mind of its own, and even technology can never truly replace a fully-functioning pancreas. Again, #weneedacure. A real cure.
“I guess if you ate low carb and had a steady line at 100 all day, dosing off of CGM wouldn’t be that bad considering the tiny boluses,” I said, shrugging my shoulders.
“Actually, I think that could be more dangerous. There’s less of a BG cushion if something goes wrong,” a doctor replied.
Very true. That, or what about the T1Ds (myself very much included), who are not always smooth sailing at 100 mg/dL all day. Sometimes you wake up with a 55, rebound up to 224 when your liver releases sugar as the juice kicks in, correct and go back down to 78, eat lunch and sit at 162 for awhile, and then somehow see a 340 by dinner because your menstrual cycle begins and unleashes hormonal hell on your body. How in the heck can we ever expect a machine to keep up with that?!!
While I have seen the argument about meter reliability, I find it a weak one. Let’s attack the issue at the root cause: meters need to improve. But, they are still a better, more immediate guide than interstitial fluid ever will be. Together, the two are a wonderful pair, showing us real-time data, trends, alarms, and so on. I am not knocking either option, but I want to ensure that I have proper access to both in the long-term.
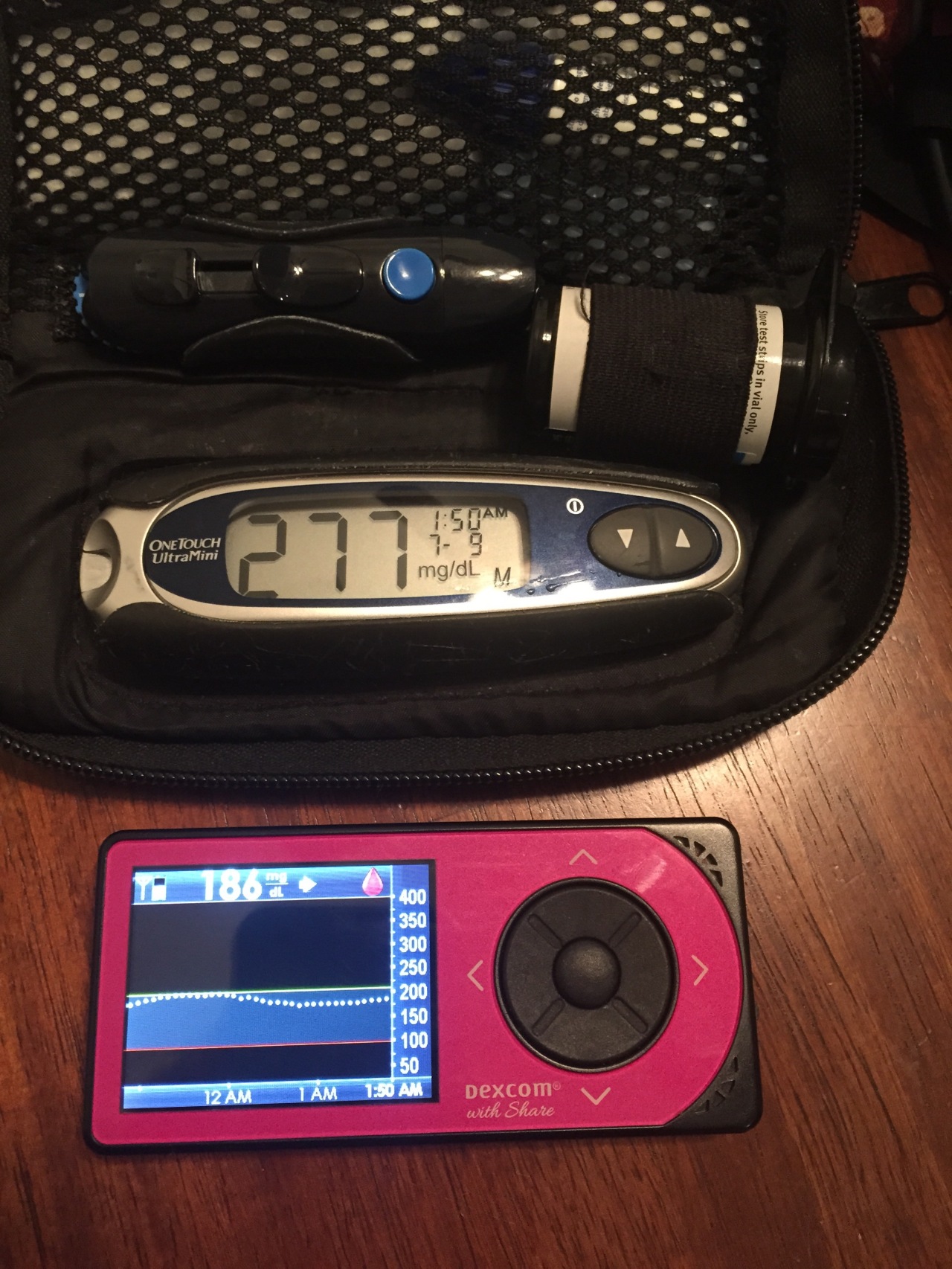
When I was normal person sick (NPS) last week, my CGM could not keep up. Neither could I, but I used all of the tools in my toolbox, to include my own diabetes intuition, to get out of the murky waters. Thankfully, I manually checked my blood sugar before dosing insulin at bedtime:

I in no way want to stifle innovation by expressing this opinion. I admire (and consider as friends) many of the advocates who are fully in support of this CGM dosing proposal. I also respect the major diabetes organizations which are onboard. Despite not agreeing wholeheartedly with their rationale in this case, I have no doubts that they want to see a better world for all diabetics. We all do, in our own ways.
My experience in healthcare leads me to believe that this decision will ultimately restrict our access to test strips, as insurance agencies will look to cut costs. And heck, as business leaders, they should; the ACA rewards and encourages cost reduction, and many consumers supported these measures vocally and at the polls. Regardless, this is beyond anxiety-provoking for so many of us. Test strips are ludicrously expensive already, and to imagine that we may be limited to a few checks a day to calibrate an imperfect CGM apparatus is maddening and disheartening, to say the least. Pass the coffee.
Imagine the current healthcare loop-de-loop. Imagine the Medtronic/UHC debacle. Actually, do not imagine- because we are already living it. And we know how unpleasant it is. Now pretend that your insurance has restricted your test strip supply, and you do not feel comfortable dosing via CGM. You have to get a letter from your endocrinologist, or perhaps a mental health care provider, indicating that you need more test strips to manage your chronic, lifelong condition which will never go away until there is a real cure. Nonetheless, you have to jump through this paperwork hoop every 3 months, missing time from work to argue with suppliers about why you need life-sustaining medical supplies. And maybe insurance will grant you 7 test strips per day instead of 2 when all is said and done… While this example is (hopefully) extreme, it is still possible. And it’s scary as heck for many of us.
“But Medicare won’t cover CGM. Or how will this affect the Libre?”
Again, I think we are attacking the wrong sources- deflecting one issue onto many others. By potentially limiting a test-strip-saavy demographic in the name of providing wider access to all is a total cop out. Instead, hold our government more accountable. CGM is a reliable tool, illustrated to be life-saving and absolutely quality of life-improving. For these reasons, Medicare folks (or swap in folks who want Libre access), deserve to have better technology on hand. But to substitute one option for another is silly, given that both CGMs and blood sugar meters have plenty of room for improvement in the current market.
Online polls and petitions do not represent the whole. From a science and data standpoint, they illustrate a sample demographic from which we can make some educated-inferences:
1.) Most of these people have computer/smart phone/internet access.
2.) This enlightens us as to their ballpark socioeconomic status.
3.) That gives us some idea of their access to and quality of healthcare.
Convenience samples are fine as long as biases are disclosed. We must say upfront that this is one side of the very large diabetes equation, and that this sample is not representative of The Whole. While we cannot all leave our fulltime jobs or school courses to lobby in front of Congress or the FDA, those representing us should be enlightened as to how we all feel, and should act accordingly.
As Erin Gilmer has respectfully pointed out on numerous occasions, there are marginalized demographics who cannot obtain the most basic of diabetes care: dental visits, for example. Yet we are up in arms over insulin pump collusion. Or, in this case, CGM dosing. The marginalized folks are not likely to be invested in this discussion because they do not have access to what is at stake; heck, they do not have access to the bare minimum. While we raise our voices, we must take caution not to further drown theirs out.
In many of the presentations of the CGM dosing issue on social media, I saw big fish in the diabetes pond introducing the topic as, “Here, this is good, hop aboard and get involved!”. This mindset is positive, for sure. But we are not whole if one of us is not heard, if different viewpoints are not given adequate opportunity to be discussed.
What about the school nurse who wrote into the debate on a Facebook status post? Did we listen when she said she would be uncomfortable dosing a child in her care at school based off of a CGM reading? Do we care?
On the flip side, if someone has great CGM accuracy and wants to lessen the finger pricks his type 1 toddler endures, am I hearing him out?
Que será, será. Whatever will be, will be. Ultimately, a decision will be made regarding the FDA and dosing with CGM. But we should all have a voice in it.
This is a long post and I surely will go to bed and realize I left out a few other big points. But this is food for thought for now. Although I am a little fish in the diabetes pond, it is my moral responsibility to use whatever platform I do have to improve life for diabetics. In my personal judgment, voicing this opinion has merit towards that cause.
I also promise to be upfront about my own diabetes biases. In the past, I have gotten on my soapbox and pledged up and down the river that we need a cure. But perhaps I have not listened to the other advocate on the soapbox next to me, who may be more focused on an artificial pancreas and who may feel that it is too painful to believe in a cure after years of disappointment. I have to respect that voice, too, because that person is part of The Whole.
So, here are my disclaimers:
1.) I can only represent my own opinions, but I hope that I can connect with others and help them by writing authentically and openly- whether we agree or disagree on various points.
2.) I will always hold out hope for a diabetes cure. Even if it does not benefit me in time, I want future generations to live in a better world. My blog focuses on this concept often, but please know that I respect everyone who strives for a better world for people with diabetes, however that world may be achieved.
3.) I will do my part to be more inclusive of The Whole. Firstly, I will feature more about cystic fibrosis-related diabetes (CFRD) on my blog. The CF community has so much to offer, and they have a valid seat at our diabetes table given CFRD/the risk of CFRD. Let’s learn more together. More to follow.
Too much skim or 2% milk leaves out a talented, diverse sample of people with diabetes. For the time-being, instead of taking my coffee very light (with cream), no sugar, I pledge to focus more on The Whole.
Thank you