This blog post serves as a simplified example of the complex headache that is the “healthcare loop-de-loop.” Ironically, I pledged to write about this topic last year as an offshoot of a blog about diabetes needles. Today, I again blog about diabetes needles, and how many hoops we must jump through to obtain minimal elements of surviving diabetes.
Many have it more difficult than me, their basic health needs unmet. Frankly, I have somewhat decent healthcare coverage through my employer, and I have also studied healthcare at the graduate level and understand its nuances. My point being: Despite all of this, healthcare remains an untamed beast, from the lower administrative levels all the way up. If I have it “good” and experience this, what about all of those slipping through the cracks merely due to circumstance?
The healthcare loop-de-loop reemerged last week when I went to refill an insulin pen tip prescription, which was promptly denied by my insurer. (I use two different types of insulin pen tips- the 4 mm BD tips for Lantus and the 8 mm tips for Humalog. My doctor and I found that the smaller Humalog volume was not being absorbed by my body with the 4 mm tips, so we begrudgingly opted for the larger 8 mm’s. Your diabetes may vary.)
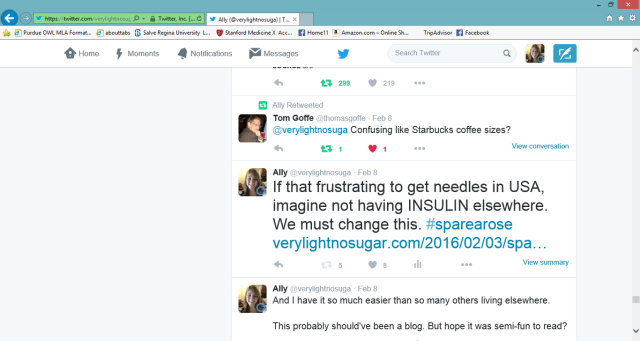
Allow me to further explain, via Twitter rant:


^ Because of the confusion about the needle length sizes and what had previously been refilled/what needed to be refilled currently, insurance flagged the new prescription as something to deny. In reality, it was simply a new prescription for a different needle length, granted by my doctor to alleviate some pain from multiple daily injections.

^ I cannot make lengthy phone calls at my job because my job duties would be compromised. And I need to work for reasons of insurance and paying healthcare bills. Many of us are in the same boat here.
^^ “This probably should’ve been a blog.” …Yup, now it is.
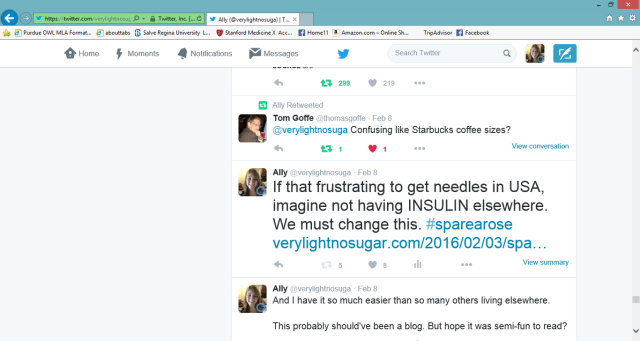
^ As maddening as this phone call marathon was, Spare a Rose puts it all in perspective. Although our healthcare situation is far from ideal in the United States, we are blessed to have what coverage we do have.
At first I felt dramatic for live-tweeting my everyday diabetes grievances. Later, I was pleasantly surprised by how many people validated my feelings, unfortunately having experienced similar irritations of their own.
The resounding theme was: This isn’t right. Whatsoever. Amen.
Healthcare is a complicated, multidimensional goliath. I just so happen to love learning about it. But when healthcare bites back at me, it is a reminder that I am still a little coffee cup in a big sea of healthcare coffee beans. Socioeconomic status, insurance coverage, and corporate power are just a few of those beans playing in the healthcare game. The stakes are high: Quality of health, and, therefore, quality of life, are on the table.
I recognize that my tiny roar may not jostle healthcare mountains. Currently, there is too much bureaucracy and red tape to allow many of my suggestions to move forward. But in order to do my part rather than sit back and complain behind the shield of my laptop screen, I must recommend some changes. If they are heard outside of the confines of my own mind, then it is worth expressing them.
I will start small, with the insulin pen tip example:
“Hi, my name is Ally. I have been type one diabetic for 25 years. One day I am confident that there will be a diabetes cure. We always keep that faith alive.
However, that cure is realistically still far away. In the meantime, I will require insulin every day in order to survive. This insulin should be affordable and accessible. Anything less is morally reprehensible. The same logic goes for any other life-sustaining medication for any other serious illness. We can and we must do better.
If a type 1 diabetic is not using an insulin pump, he or she requires insulin syringes or insulin pens (glorified insulin syringes for ease of user experience). Insulin will be delivered into the body through a needle at the end of the syringe or insulin pen.
Because I require insulin to live, and because I use injections rather than an insulin pump to manage my blood sugar, my skin must be pierced by needles every day until I am cured. Insurance could make this more bearable by not causing obviously-necessary prescription refills to be a royal pain in the @$$.
The Endo clinic could edit their coding system, so that pen tips can be ordered by millimeters, rather than gauge. No one likes to say, “Can I refill this 0.99784567325 X 54321 infinity pen tip needle, please?” Just say 4 mm in your system. Thumbs up emoji.
Kindhearted pharmacist who empathized with my worries over the insurance-endocrinology clinic ping pong battle deserves a coffee on my dime. So does insurance representative who patiently worked through the mix-up in order to get my supplies.
Understandably, BD does not want to market their insulin pen tips as “8 mm LARGE, will leave giant bruises; 5 mm semi-large, still may bruise; or 4 mm, smaller but you’re still jabbing yourself with a needle!!”. However, calling the pen tips “Short (8 mm), Mini (5 mm), and Nano (4 mm)” all indicate “small” in the minds of patients, providers, insurers, and pharmacists. You can see the root of the miscommunication.
Below is a color-coded chart, created by yours truly, for future reference. Feel free to disseminate to all parties involved here. It will lessen monthly Advil bills.
BLUE = 8 mm “Long needle. Only intended for use by badasses.” Lamely called “Short” in real life.

PURPLE = 5 mm “Medium-length needle. Sassy.” Lamely called “Mini” in real life.

GREEN = 4 mm “Small. Dainty needle for dainty pain.” Lamely called “Nano” in real life.

ALLY = happy that you listened

Thanks for hearing me out. Until the next prescription refill…
XOXO,
Ally”